If you’re reading this it’s possible you or someone close to you may be suffering from a drug use disorder. If that’s not the case, maybe you’ve seen drug abuse depicted on your television, internet or on magazine covers, especially the National Enquirer, when you’re in line at the grocery store. Regardless of the source have you ever thought, even for a second, that a drug use disorder is the result of an individual weakness? It seems that people most often view drug use problems as a nuisance because of the path of destruction a drug user leaves in his or her wake. That can include stealing, lying, assaulting someone for things of monetary value and a litany of other behaviors to have their drug use needs met. We mustn’t forget that a drug use disorder is a disease. I repeat. A drug use disorder is not a weakness, it’s a disease.
When we hear the word “disease”, we often think cancer, diabetes, heart disease and the like. Suppose your friend develops cancer after years of engaging in unhealthy behavior such as minimal physical activity, poor eating habits and tobacco use. Would you recommend sending that friend to a 28 day facility with the expectation that the disease dissipates in that period of time with zero chance of a recurrence? Unfortunately, that’s a common perspective people have about drug use disorders. Everyone wants to say, “Just go cold turkey!” It certainly is easy to say especially when you don’t have an understanding just how difficult it is to overcome addiction.
So, who’s responsible for detecting drug use disorders and how should that be pursued?
 A recent ASAM survey of two-thirds of U.S. medical schools found that they require less than an hour of addiction treatment education. That’s scary considering we lost 55,000 people to drug overdoses in 2015. Should a practitioner lack the training to properly assess for and treat a drug use disorder, which seems likely, The American Academy of Addiction Psychiatry (AAAP) has a tool to query for providers of varying levels of education equipped with the skills to complete a proper assessment in order to determine an appropriate level of care.
It is clear we have a raising problem in America when it comes to drug and alcohol use. Why not ensure the safety and care of those we love when it comes to assessment and treatment? Health care professionals need to acknowledge they are holding someone’s life in their hands and they must educate themselves on how to properly treat and care for each individual. There are no excuses, as the resources which are available to them are endless. Every single life is important.
A recent ASAM survey of two-thirds of U.S. medical schools found that they require less than an hour of addiction treatment education. That’s scary considering we lost 55,000 people to drug overdoses in 2015. Should a practitioner lack the training to properly assess for and treat a drug use disorder, which seems likely, The American Academy of Addiction Psychiatry (AAAP) has a tool to query for providers of varying levels of education equipped with the skills to complete a proper assessment in order to determine an appropriate level of care.
It is clear we have a raising problem in America when it comes to drug and alcohol use. Why not ensure the safety and care of those we love when it comes to assessment and treatment? Health care professionals need to acknowledge they are holding someone’s life in their hands and they must educate themselves on how to properly treat and care for each individual. There are no excuses, as the resources which are available to them are endless. Every single life is important.
 The justification for seeking providers outside of your physician’s ten to fifteen minute overall health check is pretty clear at this point but let’s add to the argument. The National Institute on Drug Abuse (NIDA) found that individuals coping with a substance use disorder are about twice as likely to have a comorbid mood or anxiety disorder. The NIDA has also found that mental health disorders can lead to drug abuse, which can only exacerbate an existing mental health condition. Instead of seeking out the appropriate treatment modality, they may just “self-medicate” with illicit and/or prescription drugs.
With a framework in place for diagnosing drug use disorders, the next logical step is to explore behavioral and pharmacological interventions, with the latter being a slippery slope due to the history of treatment providers using less damaging drugs (i.e. marijuana, morphine, suboxone) to treat drug abuse, which has historically backfired. Pharmacological interventions need to be closely monitored in order to ensure the prescribed medication isn’t being abused.
Several modes of therapy have been utilized in the treatment of drug use disorders with the primary modalities being Cognitive Behavior Therapy (CBT) and Motivational Interviewing (MI). In a study published by the National Center for Biotechnology Information (NCBI), CBT demonstrated sufficient efficacy with drug use treatment. While no intervention will be perfect with a 100% success rate, one study found that CBT produced clean drug screens in 60% of patients at a 52-week follow-up with patients formerly struggling with cocaine dependence.
Cognitive Behavior Therapy often employs several internal and external reinforcement strategies to prevent relapses. One external reinforcement strategy such as using prizes of low monetary value for clean drug screens has proven to be efficacious. Think back to the aforementioned idea about drugs activating the reward center in the brain. The same can apply to the rewarding feeling for engaging in healthy behavior. CBT also employs techniques that encourage internal reinforcement such as completing a functional analysis with a patient around certain cues for drug use. For example, a patient may work with their provider on identifying specific cues in the home or community that have often led to drug use such as a group friends or a specific watering hole.
CBT’s main element is to retrain the brain and create new pathways that will result in responding to foresight rather than impulse thus being fully informed of what’s about to come and a higher likelihood of positive behavior. If a patient is trained to associate thoughts about the potential repercussions of reengaging in those contexts that more often than not have lead to relapses, the patient will have an increased ability to effectively weight out the pros and cons beforehand. While the idea of CBT may sound similar to training a dog, you’re not very far off. CBT aims to reinforce positive behavior and diminish negative behavior that often results in harm. We try to teach our dogs not to run in the road, jump down from high places or eat out of the garbage because those behaviors are objectively harmful, just like using cocaine or opioids on a daily basis.
CBT doesn’t just aim to extinguish poor habits because, without drug use, something needs to be done with that extra time. A behavioral intervention of that nature encourages the client to engage in healthy activities that possess decreased risk of being exposed to an environment likely to encourage drug use. For example, a patient may be encouraged to volunteer at an organization that’s congruent with their personal interests or to exercise more often as exercise releases endorphins in the brain that stimulate the reward center. Have you ever felt that happy, excited feeling after a brisk walk, light run or hike up a mountain? That’s the result of your body responding to exercise and releasing chemicals in areas of the brain that were formerly activated by drugs to make you feel good.
The justification for seeking providers outside of your physician’s ten to fifteen minute overall health check is pretty clear at this point but let’s add to the argument. The National Institute on Drug Abuse (NIDA) found that individuals coping with a substance use disorder are about twice as likely to have a comorbid mood or anxiety disorder. The NIDA has also found that mental health disorders can lead to drug abuse, which can only exacerbate an existing mental health condition. Instead of seeking out the appropriate treatment modality, they may just “self-medicate” with illicit and/or prescription drugs.
With a framework in place for diagnosing drug use disorders, the next logical step is to explore behavioral and pharmacological interventions, with the latter being a slippery slope due to the history of treatment providers using less damaging drugs (i.e. marijuana, morphine, suboxone) to treat drug abuse, which has historically backfired. Pharmacological interventions need to be closely monitored in order to ensure the prescribed medication isn’t being abused.
Several modes of therapy have been utilized in the treatment of drug use disorders with the primary modalities being Cognitive Behavior Therapy (CBT) and Motivational Interviewing (MI). In a study published by the National Center for Biotechnology Information (NCBI), CBT demonstrated sufficient efficacy with drug use treatment. While no intervention will be perfect with a 100% success rate, one study found that CBT produced clean drug screens in 60% of patients at a 52-week follow-up with patients formerly struggling with cocaine dependence.
Cognitive Behavior Therapy often employs several internal and external reinforcement strategies to prevent relapses. One external reinforcement strategy such as using prizes of low monetary value for clean drug screens has proven to be efficacious. Think back to the aforementioned idea about drugs activating the reward center in the brain. The same can apply to the rewarding feeling for engaging in healthy behavior. CBT also employs techniques that encourage internal reinforcement such as completing a functional analysis with a patient around certain cues for drug use. For example, a patient may work with their provider on identifying specific cues in the home or community that have often led to drug use such as a group friends or a specific watering hole.
CBT’s main element is to retrain the brain and create new pathways that will result in responding to foresight rather than impulse thus being fully informed of what’s about to come and a higher likelihood of positive behavior. If a patient is trained to associate thoughts about the potential repercussions of reengaging in those contexts that more often than not have lead to relapses, the patient will have an increased ability to effectively weight out the pros and cons beforehand. While the idea of CBT may sound similar to training a dog, you’re not very far off. CBT aims to reinforce positive behavior and diminish negative behavior that often results in harm. We try to teach our dogs not to run in the road, jump down from high places or eat out of the garbage because those behaviors are objectively harmful, just like using cocaine or opioids on a daily basis.
CBT doesn’t just aim to extinguish poor habits because, without drug use, something needs to be done with that extra time. A behavioral intervention of that nature encourages the client to engage in healthy activities that possess decreased risk of being exposed to an environment likely to encourage drug use. For example, a patient may be encouraged to volunteer at an organization that’s congruent with their personal interests or to exercise more often as exercise releases endorphins in the brain that stimulate the reward center. Have you ever felt that happy, excited feeling after a brisk walk, light run or hike up a mountain? That’s the result of your body responding to exercise and releasing chemicals in areas of the brain that were formerly activated by drugs to make you feel good.
Addiction Is a Disease
According to the American Society for Addiction Medicine (ASAM) an addiction to drugs is characterized by:- Inability to consistently Abstain
- Impairment in Behavioral control
- Craving; or increased “hunger” for drugs or rewarding experiences
- Diminished recognition of significant problems with one’s behaviors and interpersonal relationships
- A dysfunctional Emotional response
Proper Diagnoses
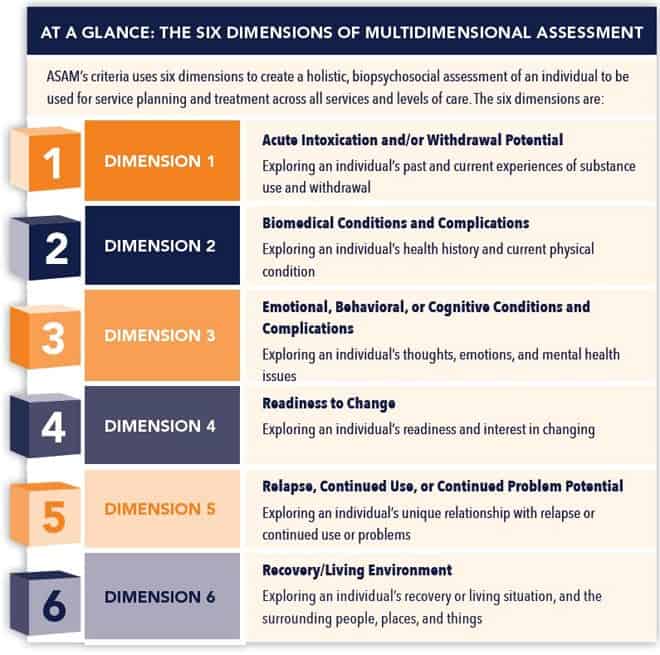
Now that we have a basic understanding of why drug use disorders should be considered a disease, what are the steps we should take to properly diagnose a drug use disorder in order to stop this epidemic? ASAM has created a set of six dimensions that can assist with determining whether an individual is suffering from a drug use disorder.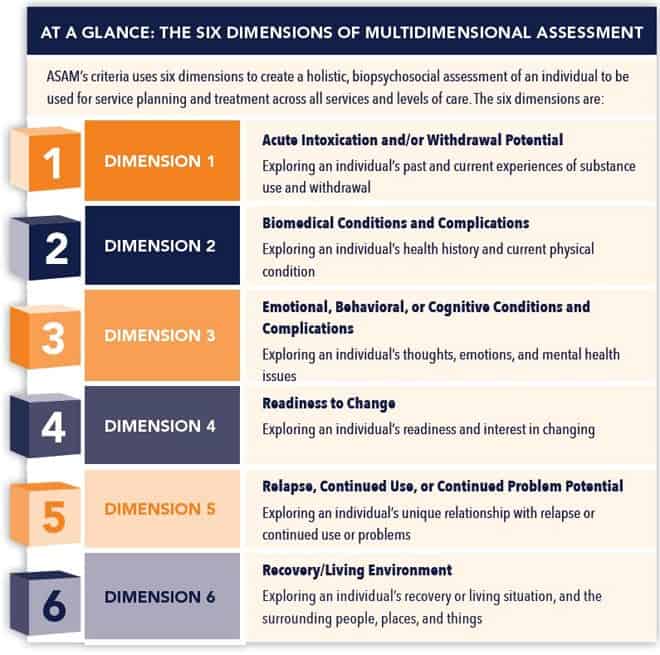 A recent ASAM survey of two-thirds of U.S. medical schools found that they require less than an hour of addiction treatment education. That’s scary considering we lost 55,000 people to drug overdoses in 2015. Should a practitioner lack the training to properly assess for and treat a drug use disorder, which seems likely, The American Academy of Addiction Psychiatry (AAAP) has a tool to query for providers of varying levels of education equipped with the skills to complete a proper assessment in order to determine an appropriate level of care.
It is clear we have a raising problem in America when it comes to drug and alcohol use. Why not ensure the safety and care of those we love when it comes to assessment and treatment? Health care professionals need to acknowledge they are holding someone’s life in their hands and they must educate themselves on how to properly treat and care for each individual. There are no excuses, as the resources which are available to them are endless. Every single life is important.
A recent ASAM survey of two-thirds of U.S. medical schools found that they require less than an hour of addiction treatment education. That’s scary considering we lost 55,000 people to drug overdoses in 2015. Should a practitioner lack the training to properly assess for and treat a drug use disorder, which seems likely, The American Academy of Addiction Psychiatry (AAAP) has a tool to query for providers of varying levels of education equipped with the skills to complete a proper assessment in order to determine an appropriate level of care.
It is clear we have a raising problem in America when it comes to drug and alcohol use. Why not ensure the safety and care of those we love when it comes to assessment and treatment? Health care professionals need to acknowledge they are holding someone’s life in their hands and they must educate themselves on how to properly treat and care for each individual. There are no excuses, as the resources which are available to them are endless. Every single life is important.
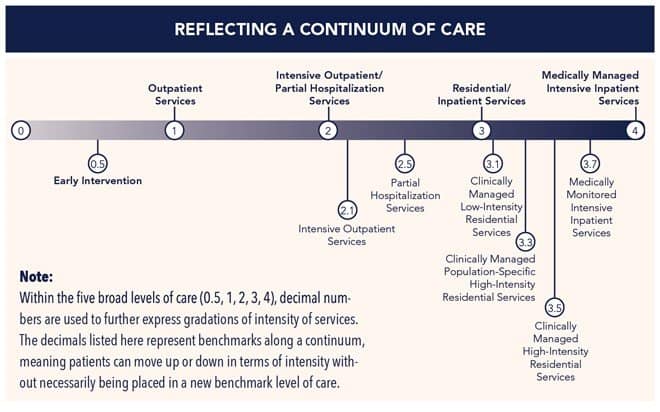
Proper Treatment
So, now practitioners know what to look for during their assessment but what levels of care will be available to the patient? No, we’re not talking insurance because that’s a completely different beast. ASAM has another trusty chart to break it down for us: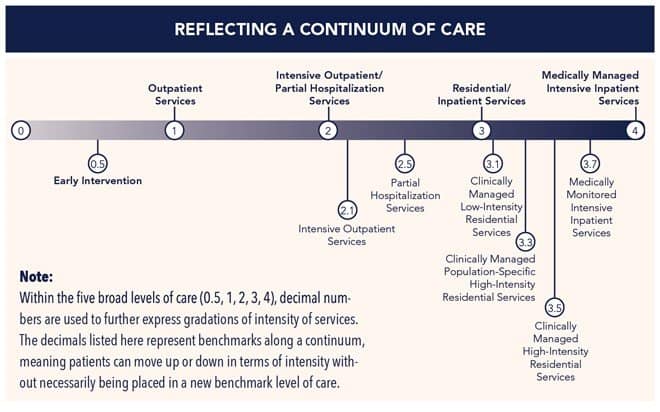 The justification for seeking providers outside of your physician’s ten to fifteen minute overall health check is pretty clear at this point but let’s add to the argument. The National Institute on Drug Abuse (NIDA) found that individuals coping with a substance use disorder are about twice as likely to have a comorbid mood or anxiety disorder. The NIDA has also found that mental health disorders can lead to drug abuse, which can only exacerbate an existing mental health condition. Instead of seeking out the appropriate treatment modality, they may just “self-medicate” with illicit and/or prescription drugs.
With a framework in place for diagnosing drug use disorders, the next logical step is to explore behavioral and pharmacological interventions, with the latter being a slippery slope due to the history of treatment providers using less damaging drugs (i.e. marijuana, morphine, suboxone) to treat drug abuse, which has historically backfired. Pharmacological interventions need to be closely monitored in order to ensure the prescribed medication isn’t being abused.
Several modes of therapy have been utilized in the treatment of drug use disorders with the primary modalities being Cognitive Behavior Therapy (CBT) and Motivational Interviewing (MI). In a study published by the National Center for Biotechnology Information (NCBI), CBT demonstrated sufficient efficacy with drug use treatment. While no intervention will be perfect with a 100% success rate, one study found that CBT produced clean drug screens in 60% of patients at a 52-week follow-up with patients formerly struggling with cocaine dependence.
Cognitive Behavior Therapy often employs several internal and external reinforcement strategies to prevent relapses. One external reinforcement strategy such as using prizes of low monetary value for clean drug screens has proven to be efficacious. Think back to the aforementioned idea about drugs activating the reward center in the brain. The same can apply to the rewarding feeling for engaging in healthy behavior. CBT also employs techniques that encourage internal reinforcement such as completing a functional analysis with a patient around certain cues for drug use. For example, a patient may work with their provider on identifying specific cues in the home or community that have often led to drug use such as a group friends or a specific watering hole.
CBT’s main element is to retrain the brain and create new pathways that will result in responding to foresight rather than impulse thus being fully informed of what’s about to come and a higher likelihood of positive behavior. If a patient is trained to associate thoughts about the potential repercussions of reengaging in those contexts that more often than not have lead to relapses, the patient will have an increased ability to effectively weight out the pros and cons beforehand. While the idea of CBT may sound similar to training a dog, you’re not very far off. CBT aims to reinforce positive behavior and diminish negative behavior that often results in harm. We try to teach our dogs not to run in the road, jump down from high places or eat out of the garbage because those behaviors are objectively harmful, just like using cocaine or opioids on a daily basis.
CBT doesn’t just aim to extinguish poor habits because, without drug use, something needs to be done with that extra time. A behavioral intervention of that nature encourages the client to engage in healthy activities that possess decreased risk of being exposed to an environment likely to encourage drug use. For example, a patient may be encouraged to volunteer at an organization that’s congruent with their personal interests or to exercise more often as exercise releases endorphins in the brain that stimulate the reward center. Have you ever felt that happy, excited feeling after a brisk walk, light run or hike up a mountain? That’s the result of your body responding to exercise and releasing chemicals in areas of the brain that were formerly activated by drugs to make you feel good.
The justification for seeking providers outside of your physician’s ten to fifteen minute overall health check is pretty clear at this point but let’s add to the argument. The National Institute on Drug Abuse (NIDA) found that individuals coping with a substance use disorder are about twice as likely to have a comorbid mood or anxiety disorder. The NIDA has also found that mental health disorders can lead to drug abuse, which can only exacerbate an existing mental health condition. Instead of seeking out the appropriate treatment modality, they may just “self-medicate” with illicit and/or prescription drugs.
With a framework in place for diagnosing drug use disorders, the next logical step is to explore behavioral and pharmacological interventions, with the latter being a slippery slope due to the history of treatment providers using less damaging drugs (i.e. marijuana, morphine, suboxone) to treat drug abuse, which has historically backfired. Pharmacological interventions need to be closely monitored in order to ensure the prescribed medication isn’t being abused.
Several modes of therapy have been utilized in the treatment of drug use disorders with the primary modalities being Cognitive Behavior Therapy (CBT) and Motivational Interviewing (MI). In a study published by the National Center for Biotechnology Information (NCBI), CBT demonstrated sufficient efficacy with drug use treatment. While no intervention will be perfect with a 100% success rate, one study found that CBT produced clean drug screens in 60% of patients at a 52-week follow-up with patients formerly struggling with cocaine dependence.
Cognitive Behavior Therapy often employs several internal and external reinforcement strategies to prevent relapses. One external reinforcement strategy such as using prizes of low monetary value for clean drug screens has proven to be efficacious. Think back to the aforementioned idea about drugs activating the reward center in the brain. The same can apply to the rewarding feeling for engaging in healthy behavior. CBT also employs techniques that encourage internal reinforcement such as completing a functional analysis with a patient around certain cues for drug use. For example, a patient may work with their provider on identifying specific cues in the home or community that have often led to drug use such as a group friends or a specific watering hole.
CBT’s main element is to retrain the brain and create new pathways that will result in responding to foresight rather than impulse thus being fully informed of what’s about to come and a higher likelihood of positive behavior. If a patient is trained to associate thoughts about the potential repercussions of reengaging in those contexts that more often than not have lead to relapses, the patient will have an increased ability to effectively weight out the pros and cons beforehand. While the idea of CBT may sound similar to training a dog, you’re not very far off. CBT aims to reinforce positive behavior and diminish negative behavior that often results in harm. We try to teach our dogs not to run in the road, jump down from high places or eat out of the garbage because those behaviors are objectively harmful, just like using cocaine or opioids on a daily basis.
CBT doesn’t just aim to extinguish poor habits because, without drug use, something needs to be done with that extra time. A behavioral intervention of that nature encourages the client to engage in healthy activities that possess decreased risk of being exposed to an environment likely to encourage drug use. For example, a patient may be encouraged to volunteer at an organization that’s congruent with their personal interests or to exercise more often as exercise releases endorphins in the brain that stimulate the reward center. Have you ever felt that happy, excited feeling after a brisk walk, light run or hike up a mountain? That’s the result of your body responding to exercise and releasing chemicals in areas of the brain that were formerly activated by drugs to make you feel good.















