Alcoholism Treatment

Alcoholism Treatment
At Arrow Passage Recovery, we understand that alcoholism is a disease that cannot be cured, only controlled. Our addiction treatment specialists understand the underlying effects of alcohol on family, friends, and health. They are trained to provide patients with the tools they need to achieve long term success through a personalized treatment program for each patient.
Our Alcohol Rehab Program
Alcohol use disorder (AUD) is a prevalent condition around the world and is linked to high-income nations where access to alcohol is easy and cheaper. In the US for instance, it is reported that more than half the American population aged 12 and above participate in alcohol use, which represents about 135.5 million alcohol users . 1 Most individuals reported the drinking as controlled. 59.7 million people reported binge drinking, and another 17 million reported heavy drinking. Effects of drinking vary from one individual to another and are determined by the amount of drinking and body composition.
At Arrow Passage, alcohol rehab treatment programs usually start with an outsourced detoxification program where the detox facility will care for you or your loved ones needs in a safe, medically supervised environment. Once detox is complete, patients move into our residential treatment center, where they partake in daily group and one-on-one counseling sessions. Therapy focuses heavily on relapse prevention, coping strategies and techniques for responding to social pressure. Patients stay with us for a period of up to 6 months, depending on their needs. For patients not requiring residential care, we offer outpatient programs.
Long-Term Recovery
After rehab, we want patients to leave us feeling confident that they’ve got the tools they need to continue to control their addiction. Our aftercare program ensures our patients are provided the support they need to remain successful and alcohol-free once they complete their alcoholism treatment. We help our patients find local support groups after returning home and continually follow up and lend help whenever needed.
Alcoholism Treatment Facilities
Our quiet, cozy 32-bed treatment facility is in Massillon, Ohio in a secluded and serene atmosphere. Our center is clean and well-maintained, and it offers patients comfortable accommodations during their stay. Our facility also features a large outdoor swimming pool that patients may enjoy during the summer months.
Defining Alcohol Use Disorders
- Drinking more than the planned amount
- Difficulty refraining from alcohol despite the need to stop drinking
- A significant amount of time is spent on getting more drinks or recovering from the previous drinking
- Alcohol craving
- Missing significant events such as work, meetings, and other scheduled events
- Continued use of alcohol despite having enough knowledge on its adverse effects
- Avoiding important activities previously engaged with in the past
Misconceptions About Alcoholism
Individuals diagnosed with alcohol use disorder often hold certain misconceptions about alcohol and about themselves, which make it hard to seek medical intervention and frequently worsen problems with alcohol. Although there is a lot of research on the impact of excessive alcohol use, many people hold specific misconceptions that may misguide decisions with alcohol and healthy living.
I Don't Even Feel Drunk
Most individuals believe that when they do not feel the impact of alcohol after a few drinks, then they do not have any issue with alcohol consumption. However, available information shows this is one of AUD’s symptoms.
Coffee Helps Hangovers
Another common misconception is that coffee can help heal from a night of heavy drinking. In reality, only time can heal a hangover.
Drink on the Weekends
Some individuals believe they do not have a problem because they only drink during weekends. However, Alcohol Use Disorders are defined by the amount of alcohol consumed, along with the frequency of consumption. Therefore, binge drinking on the weekends may still indicate a AUD.
I'm Not the Right Age for a Drinking Problem
The belief that older individuals or young adults do not have a drinking problem. However, an AUD can affect any individual regardless of age.
I Only Drink Wine or Beer
Another misconception is that one does not develop AUD because they only consume beers and wine. However, these drinks contain alcohol and are just as addictive as other types of alcohol, thus having the potential to progress into problem drinking. Additionally, the use of wine to relieve stress or fit in a group is a sign of alcohol use disorder. The inability to stop drinking after having a significant amount of drinks is also a sign of alcohol use disorder.
Prevalence of Alcohol Use Disorders
Alcohol use is a common issue among adolescents and adults in the USA. The trend of alcohol use among youth and young adults presents a worrisome trend that calls for urgent strategies to address the issue.
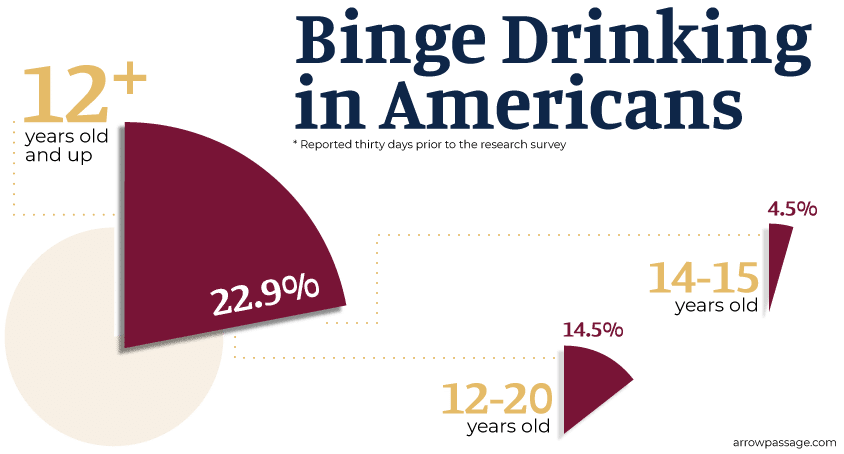
As of 2013, about 60.1 million Americans (or about 22.9% of Americans) aged 12 years and above reported binge drinking thirty days prior to the research survey. Moreover, out of those 12 to 20 years old, about 14.5% report binge drinking. Furthermore, about 0.8% of 12-13 year olds and 4.5% of 14-15 year olds reported binge drinking.
This data presents worrisome evidence among young people, more especially adolescents. Alcohol use usually increases when individuals join high school. Alcoholism can frequently be traced to developmental stages among children as they enter adolescence.
Causes of Alcohol Use Disorders
Some people have a preference for alcohol use over other groups of people. For instance, alcohol use can be traced within certain families and specific genes are linked to problematic use of alcohol. Individuals with siblings or one or more parents with a alcohol use disorder are four to five times more likely to present alcohol use issues.
There is significant research that addresses the role of genetic in alcoholism. However, there is great complexity in identifying genetic variants involved in alcohol use disorder. Historically, genetic findings have largely remained focused on specific genes.3 However, current research has had significant insight into the role of specific phenotypes related to alcoholism along with genetic influence.
Other causes of alcohol use disorder can be traced to:
- Early regular consumption of alcohol
- Peer pressure where individuals are influenced into drinking
- Using alcohol in an effort to improve moods
Consequences of Alcohol Use Disorders
Research has been essential in highlighting the toxic consequences of alcohol. Alcohol use disorders are associated with gastrointestinal, cardiovascular, immune and psychological system defects.4 Severe effects related to AUD’s depend on an individual’s genetic background, their health condition, age factor, and body mass.
Chronic alcohol use has the potential to result in multi-systematic conditions as those observed in diabetics. Moreover, AUD can cause significant damages to organs such as the heart, liver, stomach, and more. Therefore, AUD has the ability to cause breast cancer among women, liver cirrhosis, kidney conditions, gastrointestinal diseases, heart failure, and hypertension.
Cancer
Research is clear about the influence of alcohol in causing breast cancer. Notably, the risk of breast cancer increases with the amount of alcohol consumed, i.e. for every drink consumed in a single day, the risk of developing breast cancer increases by 7%. Additionally, the consumption of 2-3 drinks in a day increases the risk of breast cancer by 20% among women. Excessive estrogen levels among women are associated with breast cancer, and alcohol consumption raises the levels of estrogen among women.
Another significant consequence of alcoholism is increased cellular toxicity as a result of ethanol metabolism, an increased accumulation of acetaldehyde which has the ability to destroy intracellular proteins, resulting in cell death as a result of apoptosis.
Liver Conditions
Excessive consumption of alcohol is connected to negative liver conditions. Excess alcohol does not metabolize in the body, resulting in the accumulation of harmful substances in the body. The liver plays an important role in alcohol metabolism. Alcohol is detoxified and excreted through oxidation. Oxidation is particularly important in ensuring that alcohol does not accumulate in the body, which can result in the death of cells.
Research is important in showing the decreased oxidation ability among women compared to men. Decreased oxidation in women explains why alcohol remains in the blood system for longer among women than men. Consequently, alcohol has the ability to cause liver cirrhosis among users, and in adverse cases, patients are likely to undergo a liver transplant.
Central Nervous System
Alcohol use disorders have the potential to alter the proper functioning of the whole brain system even though the damage differ from one person to another. Excessive consumption of alcohol is linked to neurological and psychological defects. Additionally, heavy alcohol consumption among pregnant women is linked to neonatal alcohol syndrome, which negatively affects child brain development.
Additionally, long-term alcohol consumption is linked to steady decline of continuous brain functioning and other mental conditions. There is a growing body of evidence connecting alcohol use to conditions such as dementia and Alzheimer’s. Some of the conditions that are linked to brain damage due to excessive alcohol consumption include memory loss and interrupted personal behavior. Damage on the right hemisphere of the brain as a result of alcohol consumption is also linked to issues in verbal problems, visual problems, and poor judgment.
Categories of Alcohol Use Disorders
Early and Moderate Withdrawal
Alcohol withdrawal symptoms are dynamic and complex, which has resulted in the need to classify symptoms in terms of severity and period of onset to enhance recovery supports.
For instance, during the early stages, withdrawal symptoms are limited to tremors, hyperactivity, and headaches. Early withdrawal symptoms can be observed about six hours after stopping drinking or decreasing alcohol intake, which lasts between 4 to 48 hours.
Moderate withdrawal is associated with visual, auditory, and tactile hallucinations, which last up to six days.
Severe Withdrawal and DT’s
Severe withdrawal is observed through delirium tremens, which can take up to a maximum of two weeks.
Seizures can also be a symptom of alcohol withdrawal. Research shows that acute seizures linked to excessive drinking occur within 48 hours after drinking ends and can be observed in approximately 90% of alcoholics. Approximately, 5% of alcoholics present repeated episodes, which may lead to epilepsy. In adverse cases, more than 50% of seizures attributed to withdrawal symptoms are related to structural brain lesions and the use of other drugs.
Alcohol Use Disorders Detox
Detoxification is an important concept in the treatment of withdrawal symptoms supervised by doctors and physicians and is the initial step in the treatment of alcohol use disorder.6 Detoxification can be carried out through ambulatory care, which involves outpatient services where the patient is required to travel to the healthcare facility for treatment, or inpatient care which requires an admission of the patient.
Detoxification is procedural and involves initial assessments, treatment, and management of acute withdrawal symptoms which include tremor, insomnia, seizures, sweating, nausea, and delirium. In most cases, medications are prescribed to help manage withdrawal symptoms.
Some of the drugs whose efficacy has been tested include Benzodiazepines such as diazepam and chlordiazepoxide, which not only reduce alcohol withdrawal symptoms but also are essential in preventing the progress of seizures. Other drugs that may be necessary include anticonvulsants for individuals with a history of seizures that are not linked to alcoholism. Most patients get better with outpatient services and only a few get admitted for long-term treatment.
Alcohol Use Disorder Treatment
Pharmacological Treatment
Pharmacological medications for AUD include benzodiazepines (BZ) which involve a class of drugs with a sedative effect. BZ are prescribed for the treatment of seizures, insomnia, and anxiety.7 Other medications include food supplements such as vitamins and folic acid to enhance general health. Other medications include those prescribed to limit alcohol cravings and comorbid conditions.Support
Although there is significant agreement on the use of pharmacological medications to address the issue of AUD, some studies have focused on other approaches, especially for patients with mild symptoms that might gain more from supportive care without pharmaceutical intervention. Supportive care involves the provision of a calm environment with limited lighting, reduced interpersonal interaction, enhanced nutrition and fluids, positive regard, and assurance.
However, supportive care is ineffective in addressing hallucination problems and seizures. Some studies have shown that about two-thirds underwent detoxification successfully through supportive care but approximately 8% were referred to for emergency care while 2.5% required inpatient services for a successful recovery.8 Inpatient care has been found 75% effective in treating individuals who do not present other psychiatric issues or any underlying medical conditions.
Although some practitioners advocate for supportive care as an effective approach for treating many individuals with an alcohol problem, there is no specific program or guideline on the steps to supportive care. Additionally, some people have highlighted the high expenditure related to supportive care because of the need for a professional throughout the period to monitor one’s progress.
Self-help groups such as Alcoholics Anonymous have also been found to be effective in the treatment and management of AUD. These groups are essential because of the assurance that one is not alone in the problem, there is no negative judgment, and that there is hope for change.
Individual Therapies
Some individuals need private individual therapies to help address the issue of AUD and manage the symptoms that come as a result of excessive alcohol use.
Cognitive behavioral therapy (CBT) is essential in addressing individual issues regarding AUD through an initial assessment of one’s beliefs, attitudes, and events surrounding AUD. The information gained from the analysis is essential in assisting the patient to come up with coping responses which are then used in the development of practical management strategies that can be used in high-risk situations as a way of preventing relapse. CBT is important in altering underlying beliefs and misconceptions about alcohol use disorder. Additionally, CBT is effective in promoting coping mechanisms which enhance an individual’s self-efficacy, which is then applied in high-risk situations. One disadvantage of CBT is that it requires a significant amount of time to train a specialist. Patients that used CBT presented positive drug adherence and had longer abstinence from alcohol compared to patients that were put on standard care.
Alcohol-related expenses are expensive to manage, with a total budget of $223.5 billion for federal, state and local governments in the USA. Despite this huge budget, alcohol-related deaths amount to about 216 lives in a single day, which translates to 79,000 deaths in a year.
Treatment of alcoholism can be difficult due to false beliefs held by individuals that use alcohol. However, once an individual realizes that they have difficulty stopping the use of alcohol, it is probably the best time to seek the services of a professional. Exhibition of the symptoms discussed in this topic is a sign that warrants the need for professionals to help in the management and treatment of AUD.
Prevention
AUD can easily be prevented through clear conversation between parents and their children on the consequences of using alcohol or drugs. Other strategies are limiting the availability of alcohol for young adults and children, and implementing rules on drinking and driving. Raising the cost and age of alcohol consumption can also play a significant role in the prevention of alcohol use among young children.Resources
- Aronson, M. D. (2019, June 23). Patient education: Alcohol use-when is drinking a problem? (Beyond the Basics). Retrieved from https://www.uptodate.com/contents/alcohol-use-when-is-drinking-a-problem-beyond-the-basics
- American Addiction Centers. (2019, June 11). Alcoholism Treatment: Addiction Signs, Causes, & Recovery Information. Retrieved from https://americanaddictioncenters.org/alcoholism-treatment
- Clapp, P., Wackernah, R., & Minnick, M. (2014). Alcohol use disorder: pathophysiology, effects, and pharmacologic options for treatment. Substance Abuse and Rehabilitation, 1. doi:10.2147/sar.s37907
- Dguzeh, U., Haddad, N., Smith, K., Johnson, J., Doye, A., Gwathmey, J., & Haddad, G. (2018). Alcoholism: A Multi-Systemic Cellular Insult to Organs. International Journal of Environmental Research and Public Health, 15(6), 1083. doi:10.3390/ijerph15061083
- Jesse, S., Bråthen, G., Ferrara, M., Keindl, M., Ben-Menachem, E., Tanasescu, R., … Ludolph, A. (2016). Alcohol withdrawal syndrome: mechanisms, manifestations, and management. Acta Neurologica Scandinavica, 135(1), 4-16. doi:10.1111/ane.12671
- McKay, J. R., & Hiller-Sturmhöfel, S. (2011). Treating Alcoholism as a chronic disease: Approaches to long-term continuing care. Alcohol Research and Health, 33(4), 356-370. doi:10.1037/11888-002
- Simons, J. S., Carey, K. B., & Wills, T. A. (2009). Alcohol abuse and dependence symptoms: A multidimensional model of common and specific etiology. Psychology of Addictive Behaviors, 23(3), 415-427. doi:10.1037/a0016003
- Grant, B. F., Chou, S. P., Saha, T. D., Pickering, R. P., Kerridge, B. T., Ruan, W. J., … Hasin, D. S. (2017). Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001-2002 to 2012-2013. JAMA Psychiatry, 74(9), 911. doi:10.1001/jamapsychiatry.2017.2161















